What happens in the body?
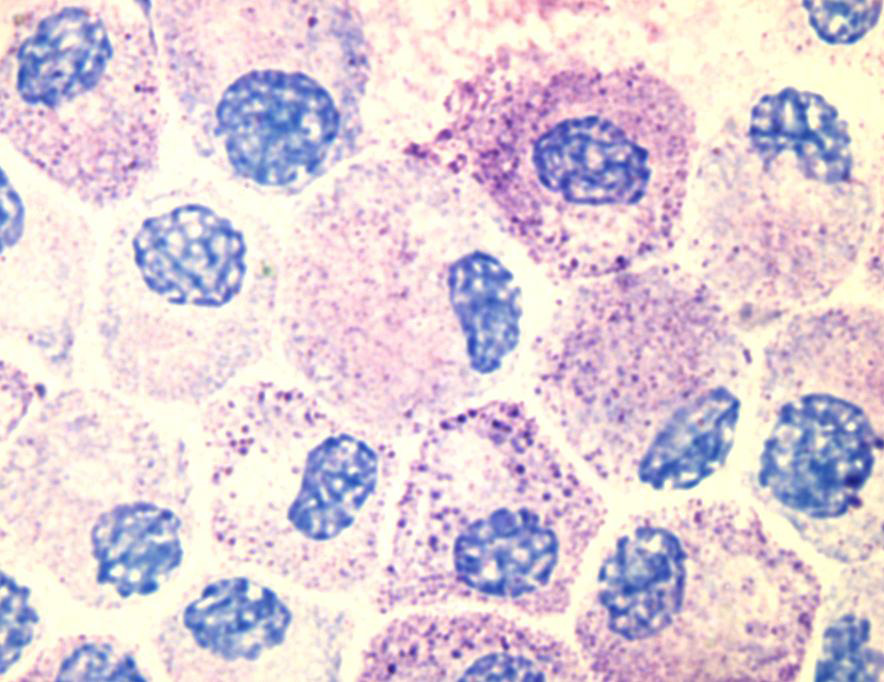
The symptoms of urticaria are triggered by inflammatory cells known as mast cells being activated. Mast cells are particularly common wherever we are in direct contact with our environment, i.e. not only in the skin but also in the mucous membranes of the gastrointestinal tract and the respiratory tract.



Different forms of wheals
Development of itching and wheals
When mast cells are activated, i.e. “annoyed” by a certain stimulus, they secrete several inflammatory substances, the best known of which is the messenger substance histamine. The release of this messenger from the mast cell causes the blood vessels to dilate and become permeable. As a result, the liquid components of the blood enter the tissue and visible wheals form on the surface of the skin. The blood vessels are squeezed by the fluid in the tissue, which is why wheals initially appear whitish. The immediately surrounding areas of skin appear reddish and are called relfexerythema in medical circles. Usually, wheals disappear within 24 hours. In some patients, wheals appear only on certain parts of the body, while in others they cover almost the entire body.
The histamine also irritates the corresponding receptors on the nerve endings located in the skin and screams “Itchy!” to the brain.
What symptoms occur?
The high number of mast cells in the skin and mucous membranes of the human body is one reason why urticaria is particularly noticeable in these areas. Activation of the mast cells in the upper (outer) layers of skin and mucous membranes causes wheals, that of the lower (deeper) layers of skin causes swelling (angioedema). Activation of the mast cells in the mucous membranes of the throat and airways can cause swallowing difficulties and shortness of breath, that of the mucous membranes of the gastrointestinal tract can cause abdominal pain, nausea and diarrhoea.
Search for triggers and causes
There are many different things that cause the appearance of acute urticaria, such as an allergy or an acute infection. However, in most cases, the cause is not easy to identify. It is different with chronic urticaria, which, according to current knowledge, is caused by autoantibodies. Antibodies are proteins that the body forms to recognise disease-causing pathogens such as bacteria and render them harmless. Autoantibodies are antibodies that are formed to target a person’s own tissues. Diseases caused by autoantibodies are called autoimmune disorders. Two different classes of autoantibodies that have disease-causing effects have been described for chronic spontaneous urticaria:
Type IgE autoantibodies
One of the types is type IgE autoantibodies. These IgE autoantibodies settle on the surface of the skin’s mast cells and activate them when the body’s own tissue they are targeting binds to them. In patients with chronic spontaneous urticaria, whose IgE is targeting their own tissues, you can also say that they have an autoallergy or autoallergic urticaria.
Type IgG autoantibodies
The second class of autoantibodies that plays a causative role in chronic urticaria are IgG autoantibodies. These autoantibodies target mast cell components and activate mast cells when they bind to them. This is referred to as autoimmune urticaria.
CSU - There are a wide variety of causes
Unfortunately, it is not possible to determine if those affected by chronic spontaneous urticaria have autoallergic or autoimmune urticaria just by looking at their skin or doing a simple test. There are also many things that influence chronic spontaneous urticaria without being the cause. These include chronic infections, intolerance to food or medication and stress. For some patients, treatment of a chronic infection, avoiding certain (e.g. histamine-rich) foods or medicines, or avoiding stress results in the urticaria improving or even completely disappearing.
Inducible forms of urticaria - the cause is clear!
It is different again with chronic inducible urticaria. Here the causes are still unclear, but it is always clear what triggers the symptoms. Those affected with chronic inducible urticaria usually know the triggers of their symptoms very well. It can also be easily confirmed by a simple test. With all inducible forms of urticaria, whatever stimulus is responsible always causes symptoms to appear each time it is present.
Which treatment is right?
With acute urticaria, a thorough investigation for triggers is usually not worthwhile. Only if there is a suspicion of the acute urticaria being of allergic nature can it be worthwhile to investigate further with allergy tests. With chronic inducible urticaria, it is worthwhile doing a further investigation of the trigger, but not an investigation of causes, as these are not known. The search for triggers must be distinguished from the investigation into causes. For this purpose, it is useful to document the symptoms regularly. In addition to the well-known urticaria calendar or diary, the CRUSE© Control App is suitable for this purpose. The investigation into causes can be helpful for severe and long-lasting forms of urticaria, but these days it is much less recommended and usually carried out at a later date than it was a few years ago. One reason for this is that today it is assumed that chronic spontaneous urticaria is caused by autoantibodies in most patients. It is not yet possible to take causal action against these autoantibodies. Its detection does not therefore mean that it would be treated differently. In other words, there are hardly any causes with such an investigation that can be eliminated by treatment. It is often very costly and an improvement in symptoms has its limits. It is therefore more expedient for patients and the doctors treating them to work on good symptomatic therapy with the aim of suppressing the onset of symptoms. These days, there is a variety of effective and safe therapies that can keep chronic spontaneous urticaria satisfactorily under control. Nevertheless, in addition to therapy, investigating the cause of severe and long-lasting cases must not be forgotten.
